Mapping Jefferson Hospital's Emergency Department
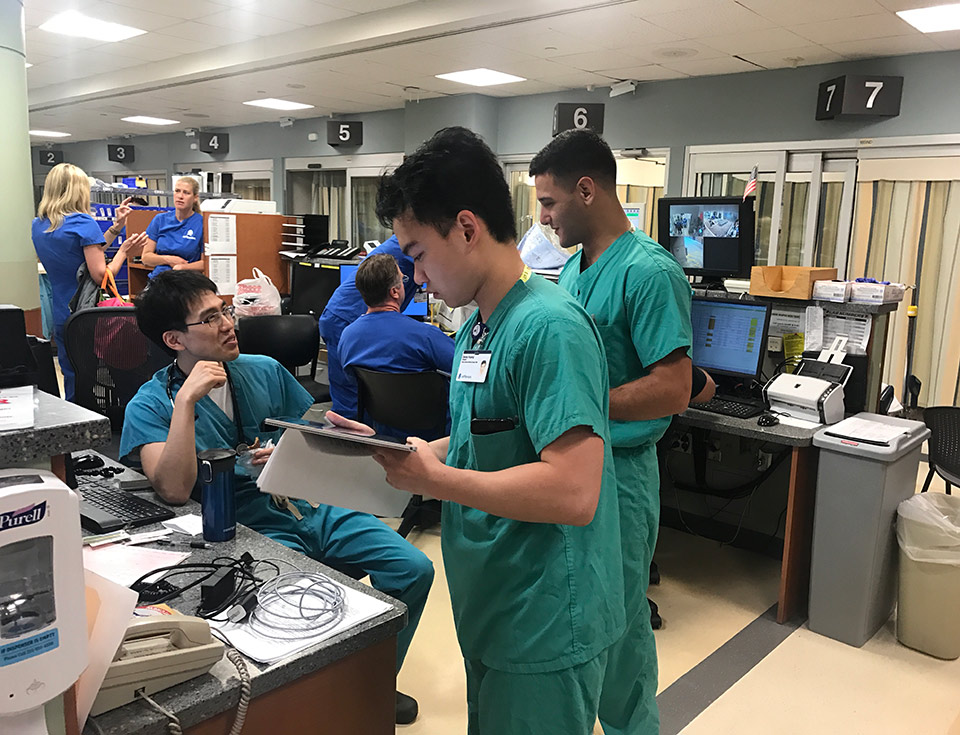
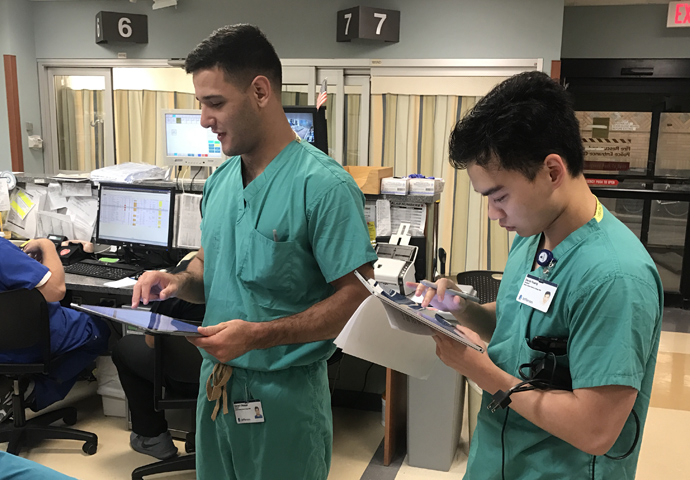
Medical students shadow ER nurses to log their movement, activity, interactions, and locations throughout a shift.
Photo courtesy of Dr. Bon Ku
This fall, our research on occupant behavior and building design made the news. In 2013, after conducting spatial survey research that explored the relationship between occupant behavior and urban park design, we began working with Dr. Bon Ku, the Assistant Dean for Health and Design and Director of JeffDESIGN at Thomas Jefferson University, to determine if this type of analysis could also be applied to the field of healthcare. In September, our resulting collaborative research was covered by the Philadelphia Inquirer. “People ask me: ‘Are you just trying to make the E.R. look prettier or polished, with the walls a more soothing color?'” Dr. Ku told the paper. “No. You can design spaces to change the behaviors of people.”
Together with a team of Dr. Ku's doctors, nurses, medical students, and hospital administrators, we used spatial analytics to investigate how workspace layout affects communication and team interaction amongst nurses and doctors in the ER department. The primary goal of our research was to uncover opportunities to introduce design thinking and innovation to emergency departments.
In collaboration with Dr. Ku and JeffDESIGN's Dr. Robert Pugulsi, we developed an occupant mapping workflow for surveyors using iPads. Over the course of several weeks, a team of medical students shadowed Emergency Department nurses throughout their shifts and used the tool to log their movements, actions, interactions, and location. We then used the questionnaire results and spatial survey data to create a rich depiction of the experience, perception, and measured behavior of nurses in the hospital.
Using research that spanned two summers, our spatial analysis helped paint a picture of the many ways patients and healthcare providers inhabit Jefferson's Emergency Department, and gave us a better understanding of the relationships between hospital layout and the behavior, productivity, and delivery of care of its nurses. In particular, our surveys focused on communication between nurses and their patients, colleagues, and staff.
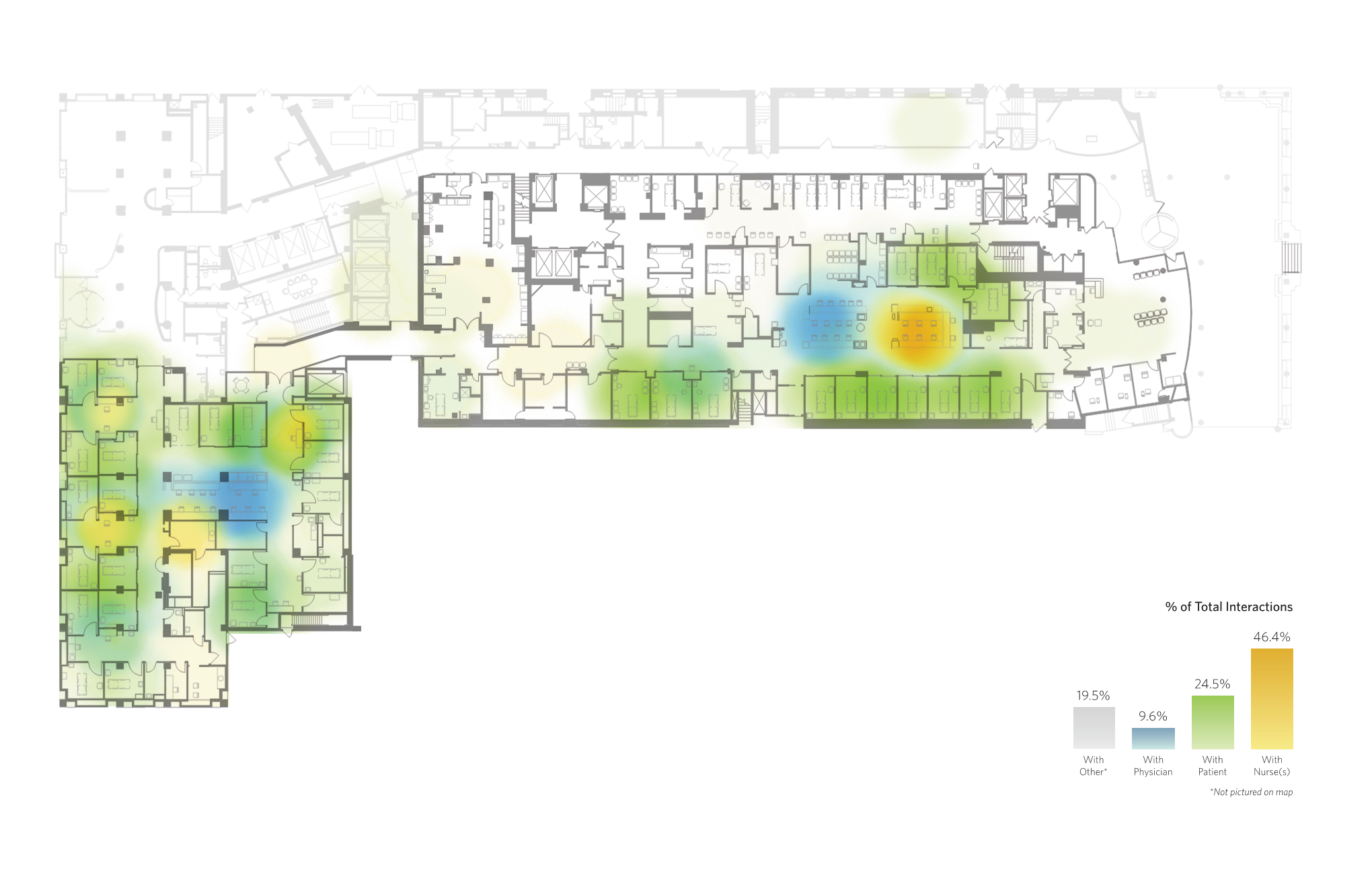
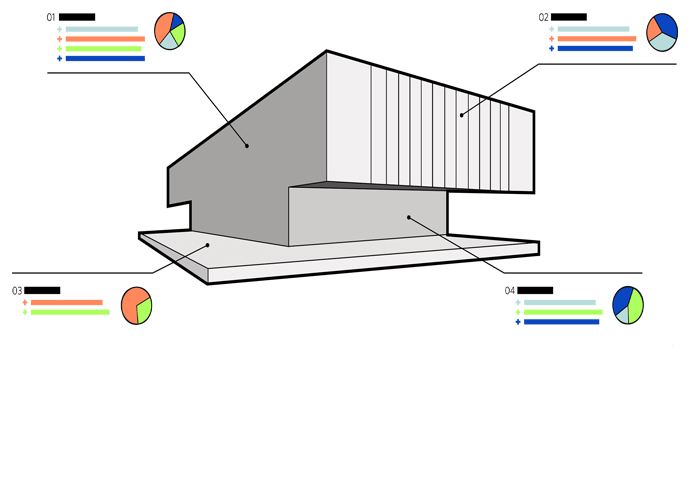
A customized survey tool allowed the team to track the movements of hospital patients and staff over time to see how the Emergency Department's layout impacted their interactions.
With a pair of distinctly organized department wings, Jefferson's Emergency Department provided an ideal backdrop for a comparative study. The A-side's centralized layout concentrates a cluster of nurses and doctors in a workstation surrounded by patient rooms, whereas the B-side's decentralized layout and individual nurse stations distances the nurses from other hospital staff in order to situate them closer to patient rooms. Many nurses and doctors voiced strong opinions about which layout they preferred and how it affected their movement and communication.
Our study revealed that on average, the B-side's decentralized layout led to increased communication and contact time between doctors and nurses despite the greater distance between their workstations. We also discovered a great deal of variation in how individual nurses moved through the space. This simple experiment has led to a deeper and ongoing analysis of other variables that affect nurses' movement and experiences, from their patients' conditions to the composition of their larger care teams. As is often the case, quantitative analysis doesn't tell the full story, but it can help the managers and designers of complex environments like a hospital emergency room unearth patterns and possibilities.
The team used the survey tool to monitor not only patient and staff locations and movement in the Emergency Department, but also who nurses were interacting with in the Department's various spaces.
Earlier this year the Centers for Disease Control and Prevention published a report outlining the startling growth of emergency room visits in the United States over the last several years. According to the CDC, one-fifth of Americans visit an ER once a year, and in 2016 alone there were 141.4 million patient visits to emergency departments across the country. Despite their financial cost, the growing rate of ER visits offers encouraging feedback that a growing number of Americans are seeking out and receiving the care they need. In other words, emergency departments are busier than ever. The question remains: how can we make them even better?